Posted by Jasmine:
My daughter, Kai, is a transplant patient.
We started receiving benefits through United Healthcare on February 1st. At the time, my husband was switching companies and our old health insurance, through Cigna, overlapped for a period of one month. My husband went 1099 with his company in August and we enrolled in COBRA to continue our benefits through United on Sept 1st. His company renewed the plan on April 1st.
I believe in July they started denying claims, saying that we had a secondary insurance (referring to the brief overlap, in which Cigna was used as the primary insurance). I called and explained that the Cigna coverage only overlapped because we had already paid for the month before my husband switched companies and that coverage ended March 1st. It appeared to be resolved but I’m not certain if it ever was. We were receiving $1,700+ bills at the time for my daughter’s routine lab checks, as well as denied claims for pediatrician visits, etc.
Next, I started receiving more denied claims stating that we hadn’t met our deductible. Normally, our deductible is met very early in the year due to my daughter’s very high, frequent medical bills. I called them and they confirmed that we had not met the deductible, went over what my deductible’s were and how much I had left to pay. Confused, I started paying those bills because I didn’t have the information to refute it – the EOBs were only online and I didn’t have the log-in information. My husband had to contact his company to get it, but the business that they contracted to administer their benefits was very difficult to communicate with.
In the meantime, they also denied authorization for a surgical procedure for my son, my daughter’s medications, forced us to go with their specialty mail-order pharmacy to get the medication that is necessary to keep her alive and then made it difficult to refill on-time with no ability to escalate to any kind of manager, consumer advocate or appeal the situation.
My family and I started posting on their social media pages and I began blogging about how they were denying us coverage that we are paying $1,200/month for. Initially, United contacted my mother and asked for my contact information. They pointed the finger at their specialty Rx devision, Optum Rx. A woman from Optum called me and told me that, though her hands are bound by United’s policies, she would do anything in her power to get Kai’s medicine to her on time, even if she had to bend the rules a bit, and gave me her direct line.
Then, my daughter was hospitalized for pneumonia for about 5 days and she was denied her medication (a tier 1 antibiotic) upon leaving the hospital. I still can’t tell you exactly why or what exactly happened on the United side with that, but the discharge nurse called the Rx (levaquin, which she had been receiving via IV and it was the only antibiotic she had responded to) to CVS. When I called to see if it was ready, they told me it would be nearly $800! I called United and they argued with me, saying it should only be $10. I agreed and the representative called the pharmacy, then she told me it wasn’t covered because they didn’t have it in stock. I then called my daughter’s old pharmacist and asked him to run it for me. He also did not have it in stock but he said it would be $60 (not $10 and not $800). After contacting my daughter’s transplant team, they decided to write her an Rx for a less expensive antibiotic and hope it worked because, at that point, she just needed to get the dose on time so the the pneumonia didn’t reestablish (being immune suppressed, it can be very serious for her).
I took to social media, again, and an executive from the United Healthcare corporate office in Connecticut in the Consumer Affairs department contacted me. She offered to be my case manager. She called back a few days later to say that she didn’t understand why my son’s surgery had been denied – that my plan should cover it – and that there was no record of any attempt to authorize it (which is false because I received a letter from them about it AND wrote a letter of appeal) and they also said there was no record of my calling about my daughter’s levaquin. She sent a letter with her number and the number for someone else if I should have trouble getting my daughter’s Rx through their mail-order pharmacy. I have not heard from her since.
Finally, I went to pay bills this weekend and realized that all of our claims are STILL being denied. I called again yesterday and they said, again, that we had not met our deductible. To which I replied, “There is NO WAY.” I asked when the deductible started and the rep told me September 1st… when we enrolled in COBRA. We didn’t change our plan, it didn’t renew, we just started paying for the benefits ourselves ($1,200/month). The deductible SHOULD have started in April, when the plan originally renewed. Further more, I know we MUST have met the deductible some time ago because we also had an HRA from his company that paid 75% of the total family deductible, that was exhausted sometime between July-September (I’m still trying to get all the info together). We would have had approximately $700 left to pay toward it and I know we’ve paid significantly more than that.
I called and left a message for the executive who was at lunch when I called around 1:40pm. She has not called back. I called the number on the back of my card again and was told that, because they can’t “see” my plan prior to September 1, I am responsible for telling them when I reached my deductible and providing them with the particulars.
So, here we are. I was finally able o get the log-in for MyUHC online and review the EOBs and it’s just a complete mess. It doesn’t look like they adjusted anything from when they were claiming we had secondary insurance. The total “Patient Responsibility” listed is over 4x’s what our annual family deductible is and we have a $21,000 claim waiting to be processed with about $500 worth of bills/denied claims waiting to be paid.
Also, we have been paying for dental coverage through United/COBRA with Guardian and, although we are up to date on payments and just received confirmation of that via mail with an itemized explanation, we were told that they are denying that we have coverage at all when I tried to schedule my kid’s dentist appointment.
I have not yet had a chance to even attempt to resolve this as I have been focusing on the medical coverage issues.”
I am a mother of 3 with a chronically/seriously (and, by some definitions, terminally) ill child. I work 2 part-time jobs from home. I homeschool my children to better take care of my daughter’s health issues. I spend an average of 8-12 hours a week on the phone, trying to get the coverage we pay for from United Healthcare. They are ROBBING my family and getting away with it.
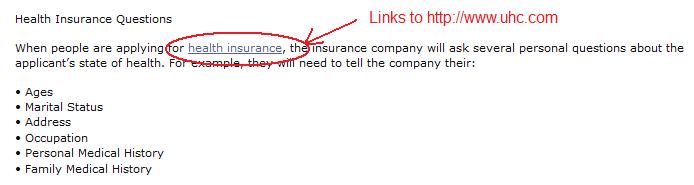
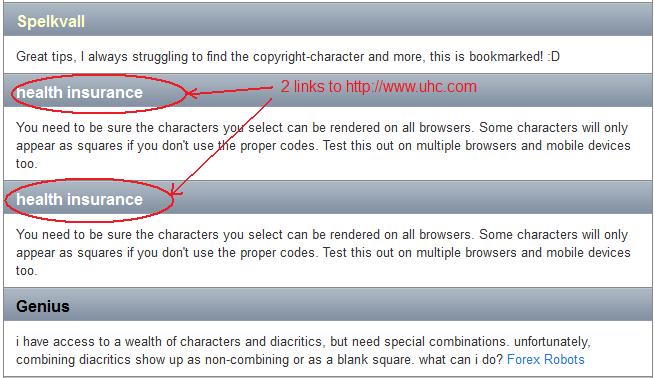
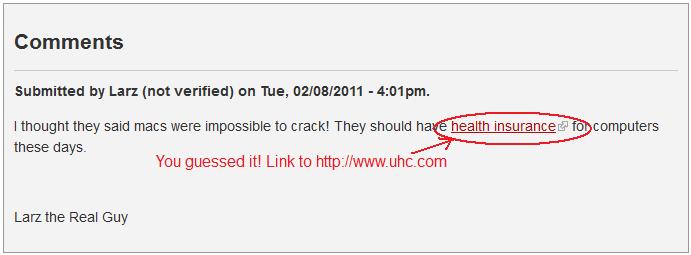
 Disclaimer: Unfortunately, it cannot be proven (unless you’re Google) whether United Healthcare, an agency working for them or someone else has done this, but it’s definitely helping UHC to rank UNFAIRLY in Search Engines! Look at my findings below and decide for yourself. I am NOT claiming that UHC did this!
Disclaimer: Unfortunately, it cannot be proven (unless you’re Google) whether United Healthcare, an agency working for them or someone else has done this, but it’s definitely helping UHC to rank UNFAIRLY in Search Engines! Look at my findings below and decide for yourself. I am NOT claiming that UHC did this!